Microdiscectomy procedure
Microdiscectomy is the minimally invasive procedure for the removal of disc herniation. It eliminates compression of the nerve root. This procedure requires only a small incision and takes 40 to 90 minutes. During the procedure, patient stays under the general anesthesia. The patient can walk on the next day after the operation. Hospital stay usually takes 7 to 9 days.
In operation room patient is put into medical sleep (general anesthesia). Surgeons put the patient in a prone position with soft bolsters to widen natural spaces between the vertebrae. Special X-ray device (electronic image converter) helps to produce spine images in the real time. Surgeon treats the place of the incision with antiseptic, creating the sterile zone, which is bordered by sterile sheets and concealed by a surgical film for retaining the sterility for the entire operation. After this preparatory work the surgery begins.
X-ray device helps to determine the level of the disc, and the surgeon uses a special pin to determine the length of the incision. The incision is usually 2-3 cm long. After gaining access to the spine, the surgeon makes another scan with the pin to check the disc level.
Then surgeon uses retraction device, which separates soft tissues and muscles so that long and thin instruments could pass into the wound. After that begins the micro-surgical procedure with the microscope.
 Figure 1. Operating room. Surgical team and equipment during the microdiscectomy procedure
Figure 1. Operating room. Surgical team and equipment during the microdiscectomy procedure
The surgical stereomicroscope provides magnification x5 to x20 and helps to distinguish the bone, cartilage, small vessels and nerves. The stereo system of modern microscope makes it possible to navigate in the wound in a fast and efficient way. Thanks to its steady base, automatic balancing and the system of optics control surgeon can accurately direct the microscope axis and regulate the magnification.
The surgeon can also use endoscope during the procedure. It is a long shafted instrument with a lens, with which surgeon can glance into the closed space and decrease the volume of the bone resection. Unfortunately, the endoscope has a monocular system. The surgeon looks into the endoscope only by one eye, sees a flat picture that lacks a three-dimensional feeling of depth.
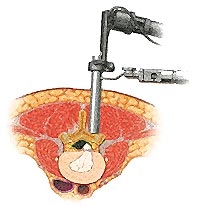 Figure 2. Endoscope in removal of disc herniation
Figure 2. Endoscope in removal of disc herniation
After the exposure of the vertebral arch вАУ by high-speed drill or Kerrison rongeurs, surgeons performs a small bone resection. It is necessary to reach the point of nerve root compression by herniation and perform safe decompression. Proper arch resection does not influence the support function of spine.
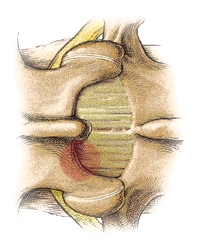
Figure 3. Resected part of the vertebral arch
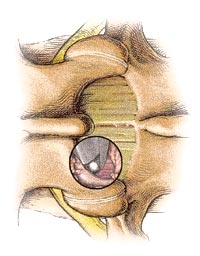
Figure 4. Vertebral arch resection with Kerrison rongeurs
After lower third of the vertebral arch is resected, the surgeon gets access to the yellow ligament - natural soft protector of nerve root. The surgeon carefully separates the yellow ligament from dura and nerve root and resect a small portion of it. Then surgeon displaces nerve root and dural sac with small and thin retractor and gets access to the herniated disc.
Usually, disc herniation looks like a small shrimp. Its shell is easily ruptured in contact with surgical instrument, and sequestered disc gets out. The surgeon uses special thin tools to find and remove the remainders of cartilage under the posterior longitudinal ligament, from the vertebral foramen and other places. After this surgeon performs curettage of the disc cavity and lateral pouch to prevent recurrent herniation.
Procedure finishes with flushing the wound with antiseptic, establishing drainage and suturing. At the end of the procedure, the patient wakes up and returns to the ward. Next day after procedure patient can walk.
Sometimes this surgery is combined with the spine fixation to strengthen the connection of two or more vertebrae. There are several techniques of spine fixation – fusion with transpedicular screws and rods or dynamic fixation (preferably in athletes and young active patients).


